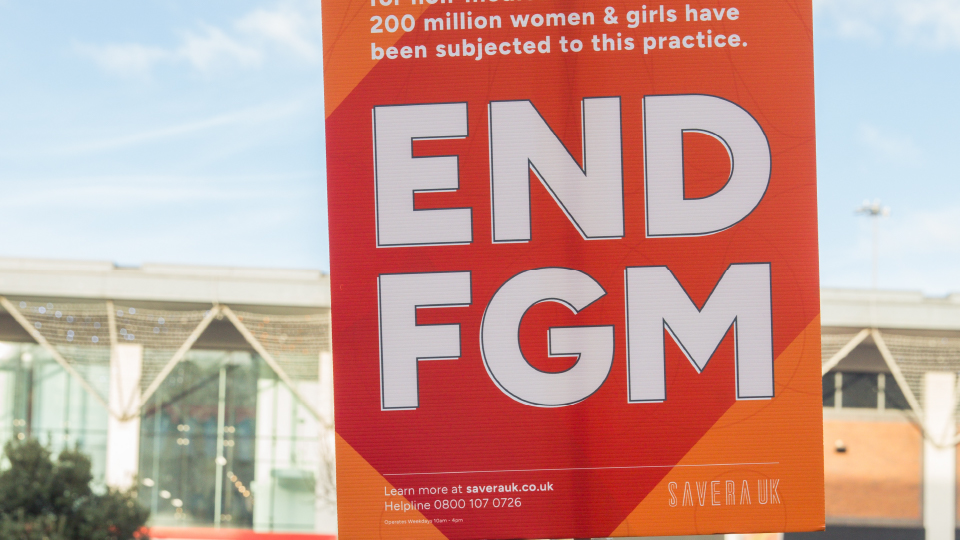
In England and Wales an estimated 137,000 women and girls are living with the consequences of female genital mutilation (FGM), and 200 million globally have been subjected to the practice, three million of those in Africa alone.
But it does not have to be this way.
Working in Kenya as a UNICEF Youth Advocate, our ‘Honour’-Based Abuse and Harmful Practices Specialist Worker, Eve, saw the direct physical and mental impacts on survivors. But she also discovered communities that had once undertaken FGM, but had since rejected the practice, which has inspired her drive to end the practice for good.
We spoke to Eve about what working in communities has taught her, how the Savera UK Direct Intervention team works with survivors, those at risk and the professionals who help them, and what we can all do to help end FGM.
Tell us a bit about yourself and your knowledge of FGM?
Before joining the team at Savera UK, I previously worked with UNICEF Kenya as a Youth Advocate. This involved me working within the Child Protection team, focusing on programmes to end harmful practices such as FGM and Child Marriage. I also worked on the UNFPA-UNICEF Joint Programme on the Elimination of Female Genital Mutilation.
My career has given me insight into working at various levels to create change, from influencing government policy to working in grassroots organisations directly with communities to change views and learned behaviours.
Whilst working in Kenya I got the chance to meet a variety of people that developed my knowledge and understanding of FGM. The most notable learning experiences for me was meeting with communities that once practiced FGM but have now changed their outlook. Meeting young survivors of FGM and seeing first hand the impact it has had physically and mentally was incredibly eye opening. This allowed me to to truly understand the issue of FGM from a much broader perspective.
What is your experience of having worked on FGM cases?
The majority of the FGM cases I have worked on at Savera UK have all ended positively. They usually include a client that is a survivor of FGM who is worried that their daughter will also be subjected to it. To ensure the clients get what they need, we work closely with other agencies, and when needed, we have been able to obtain an FGM Protection Order (FGMPO). An FGMPO is a family court order that protects someone at risk of FGM, but it does not criminalise a perpetrator unless they break the order. This isn’t something that we do, or is applicable to all FGM cases, and sometimes it is not what the client wants. However, it is a powerful tool that we have available to help people, if it is the right thing for them and their specific circumstances.
In these cases, the potential risks and signs of FGM are often picked up by healthcare professionals and so the clients that are survivors of FGM are able to access specialist advice in relation to the type of FGM they have experienced. It is common for survivors of FGM to experience trauma as a result of this invasive practice. Savera UK offers specialist trauma informed counselling so they can begin to heal mentally as well as physically.
What signs should people look out for?
There are many potential signs that could indicate FGM, but it is important to note that all cases are different and do not follow a specific pattern. Due to the different types of FGM, some individuals may not know that they have been subjected to FGM or even be aware what it is.
Some indicators that FGM may be taking place, might include a planned trip to a country where FGM is prevalent, history within the family of FGM and/or from a community that practices it and conversations around special ceremonies/occasions.
Indicators that it has already happened may include a reluctance to undergo medical examinations, withdrawal and change in behaviour after a long absence, spending longer in the bathroom and persistent urinary or menstrual problems.
What advice would you give to a member of the public who thinks they know someone who might be at risk of FGM but is unsure what to do, or too nervous to come forward?
Sometimes people might be nervous to come forward as they are fearful of the repercussions. This fear can be due to a lack of understanding or being taken seriously by professionals, not wanting to offend others or be accused or stereotyping. If you have worries that someone is at risk of FGM, do not discuss this in front of family members that could be complicit in arranging or carrying out the practice. It is best to highlight these concerns to someone outside of the community or family. The best advice I can give to someone who has concerns is to contact a trusted professional. This could be a healthcare professional (GP/Nurse), teacher or children’s services. All these professionals and agencies will have protocols and safeguarding procedures and should investigate the concerns. Any reports made to professionals will be treated confidentially so individuals do not have to worry about coming forward.
If you are unsure whether a person is at risk of FGM but have any concerns at all, you can call our helpline and we will provide the best advice on the next steps to take. Even as a member of the public, the ‘One Chance Rule’, should be followed at all times, so it is best to take action as this could be the only chance to prevent FGM from occurring.
What can someone do if they are in a different country and they aren’t a British citizen?
There are many organisations in different countries that can provide advice to those that have experienced or are at risk of FGM. Some of these organisations are Womankind, End FGM EU and Forward.
Although there are laws prohibiting/criminalising FGM in many countries in the world, unfortunately contacting the police isn’t always a viable option for individuals. Police services in other countries do not offer the same support as we do in the UK, although it is illegal it isn’t always enforced. This is a wider problem that needs to be addressed. There cannot be a global aim to end FGM while some countries do not criminalise the practice.
If people come from a country or community that practices FGM, it is always important to be an advocate against the practice where appropriate. Educating others and talking about the risks and implications of FGM is vital to the global effort of ending FGM.
What is something you have learned about FGM that surprises people when you tell them?
FGM is a practice that is controlled and influenced by elders in communities. Although parents and other relatives may not want the girls in their family to undergo FGM, it may still be enforced by the wider community and parents will have no say in this. This can become complicated when trying to protect children at risk of FGM as there are multiple perpetrators to consider, as well as the parents to guide through external pressure.
How does the Savera UK Direct Intervention team help someone at risk of FGM?
The intervention provided to someone at risk of FGM is different in every case, and subject to on the needs of the client. Our intervention begins with a referral. This can come from a professional that may have concerns that the client is at risk or a survivor. Individuals are also able to make self-referrals into the DI team, through our website, if they have experienced FGM or believe they/or someone else is at risk of FGM.
From this we conduct a risk assessment to further understand the experience and risks of the specific client. This enables us to create a plan of action and contact the most appropriate agencies. Throughout this process a client’s confidentiality is maintained at all times unless they are at immediate risk of harm, and we work to ensure the client’s voice and wishes are always heard.
At the end of the day, we are there to represent our clients – to always advocate for them and help them to find their new beginning.
If you or someone you know may be at risk of female genital mutilation (FGM) contact Savera UK’s helpline on 0800 107 0726, open Monday-Friday, 10am-4pm. If the risk is immediate, call 999. You can also refer someone else or make a self referral online using the links provided.